“I’ve had a couple of different careers before this” says Natalie Loops, MSN, RN, CNL.
“I’ve had a couple of different careers before this” says Natalie Loops, MSN, RN, CNL.
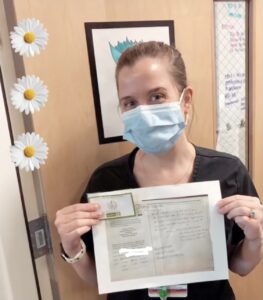
She is now a clinical instructor at Rush University, but she took a path less traveled to get there.
After graduating with a degree in biology from the University of Illinois-Chicago, Natalie knew she wanted a career in healthcare, but she wasn’t exactly sure where. She went to medical school for a year (in the Caribbean!) before deciding that wasn’t quite the right profession.
She decided to become an MRI technologist instead. She enjoyed it, but then a long commute had her applying to a health care consulting company where she became a certified medical coder and eventually medical coding consultant associate.
It was during this time when she realized, “I was happiest in my life when I was with the patients, even for that little bit of time when I was an MRI tech … I like being that person to help them,” says Natalie.
While working as a medical coding consultant she volunteered at Northwestern Medicine on the neurology floor. This experience solidified her decision to become a nurse. Natalie enrolled in Rush University’s general entry MSN program. She worked as a nurse’s aide in the Neurological IMCU at Rush while studying and was hired upon graduation.
Working on Rush’s Neuro IMCU Floor
With patients with a variety of conditions—from strokes and brain tumors to Parkinson’s, dementia, and Creutzfeldt-Jacob disease—no two days or two patients were alike. “There’s something different every single day. It’s never the same on that floor. I like that. I like the excitement.” Natalie goes on to say she is fascinated by the minds of those that help create this ever-changing environment and she is attracted to learning about this constantly evolving field.
The mental health aspect of the work of nursing on the neurology floor also appealed to her. “I think neuro often gets classified in a med/surg capacity, but it’s very much psych, too.” Nursing this population involves providing constant mental health care.
She did that in a variety of ways that demonstrate her compassionate and individualized care for patients.
“Some people want you to listen and try to be there for them. Some people want the least amount of stimulation possible, and you just try to cluster your care so you can do as many things at once when you’re in there,” she explains. “Sometimes it’s family” that also need assistance.
Within her scope of practice, she requests additional support, to provide the best care possible for her patients. “At Rush, we can put in orders for the chaplain, music therapy, and a nurse psych liaison” to assist with helping the patients achieve optimal mental health.
In everything she does, she brings empathy and empowerment to patients.
“For those who are scared, which is a lot of people on the floor, I make a very conscious effort of letting them know exactly what I’m going to do before I do it, even if it’s something that seems so common to me like a blood pressure: ‘Hey, I’m going to reach for your right arm right now. I’m going to wrap this blood pressure cup around it, ok? It’s going to squeeze. Alright, here comes the squeeze.’ She tries to have no surprises and give reassurance of what is going on.
While ill and in an acute care center people feel like they lose their ability to have control. So, I do a lot of: ‘Ok, we can do an assessment first or we can do meds first. What do you want?’ or ‘I need to get this done in the next half hour. Do you want me to come back, or can we do it now?’ Giving patients choices enables them to have control. She also tries to educate as much as possible, so patients understand what is happening to them and how tests and procedures are done. This tends to alleviate fear and allow a patient to take an active role in their healthcare.
She says her nursing abilities are a work-in-progress, “I think my people skills are constantly developing.”
Teaching & Starting Her DNP
Now, she’s transitioning into another position. Recently Natalie started as full time faculty at Rush University College of Nursing.
She enjoys watching students become more confident and skilled in such short periods of time.
For the past two semesters Natalie was a clinical instructor for the nursing students first medical surgical experience. “It’s such a fun semester because they start out really insecure about even doing care like vital signs or ambulating patients. Then, by the end of the semester, they’re going over meds; they know why the patients are getting these interventions, and they’re educating patients. It’s cool. It’s fun to watch them grow.” “I really like it. I like being part of that.”
As a lifelong learner, Natalie is currently working on her DNP at Rush University. She’s specializing in psychiatric and mental health. Her love of neurology and psychology began twenty years ago when she was involved with serotonin research in undergrad. It continued as she imaged patients’ brains and helped her grandparents with dementia, and it reached an irreversible momentum when she was working as a neuro nurse. She loves how neurology and psychology overlap and she becomes enthusiastic when talking about all the “new exciting” developments in this area.
Working for the Wellbeing of Nurses
Natalie’s interest in mental health extends beyond the patient and to her fellow nurses as well. How can we better help the helpers, especially after a distressing event on the job? She’s planning to use her time in the DNP program to explore more ways to support nurses.
When asked how she wants to use this education once graduated she states, “I am very interested in healthcare workers’ burnout, so if there’s some way, I could help with that – I would love to have that opportunity. It seems like a great way to feel like you helped people at the end of the day.”